Ease Menopausal Joint Pain with These Supplements
Get relief from menopausal joint pain with our list of the best supplements for joint pain menopause. Discover top menopause joint pain relief options.
BONES & BODY WEIGHT
ActiveVitaLife
4/10/20257 min read
Estradiol, a type of estrogen, helps protect muscles and bones. When levels drop, many notice stiffness or achiness. While activity and diet influence severity, finding relief is possible with the right approach.
Key Takeaways
Over half of women face joint discomfort during hormonal shifts.
Estrogen decline contributes to inflammation and bone loss.
Lifestyle factors like diet impact symptom severity.
Professional consultation ensures tailored treatment plans.
Integrating natural and medical options offers comprehensive relief.
Understanding Menopausal Joint Pain
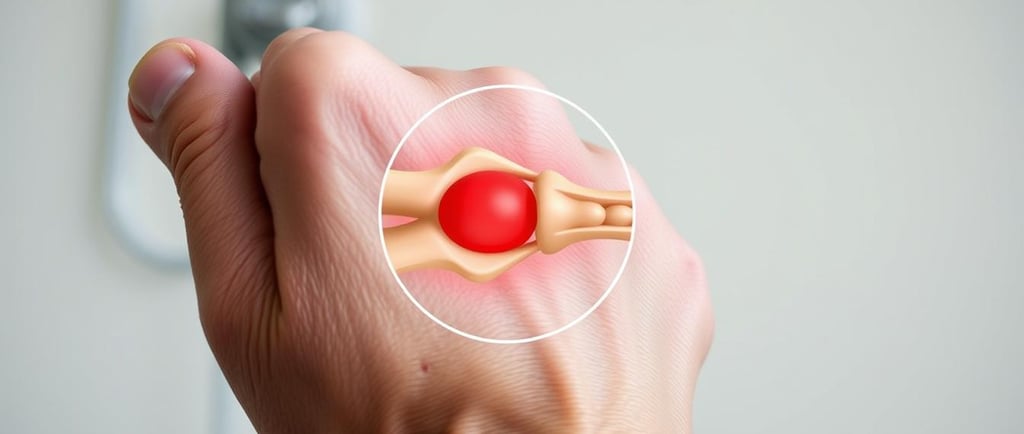
Many women notice increased stiffness as hormonal shifts occur. This discomfort stems from complex interactions between hormones and tissues. Estrogen, for example, helps maintain cartilage and synovial fluid, which cushion joints.
Why Hormonal Shifts Trigger Discomfort
Declining estrogen levels heighten inflammation and reduce bone density. Cartilage loses protection, leading to friction and stiffness. Weight gain adds stress, while muscle loss (sarcopenia) weakens joint support.
How Changes Affect Joint Health
Fluctuations raise osteoarthritis risks, especially in knees and hips. Losing just 10% of body weight can ease knee pressure significantly. However, long-term NSAID use (like ibuprofen) may harm kidneys or liver.
Key takeaway: Addressing root causes—like inflammation or muscle loss—offers more relief than masking symptoms. Always consult a doctor for persistent issues.
Top 9 Supplements for Joint Pain During Menopause
Hormonal changes can lead to discomfort, but certain natural options may help. Research-backed ingredients target inflammation, cartilage health, and mobility. Below are nine science-supported choices worth considering.
1. Turmeric (Curcumin): Nature’s Anti-Inflammatory
Turmeric’s active compound, curcumin, reduces swelling and stiffness. A 2021 meta-analysis of 10 studies confirmed its benefits for knee health. Dosages of 500–1500mg daily showed notable improvements.
2. Omega-3 Fatty Acids: Fish Oil for Joint Lubrication
These healthy fats combat inflammation and support fluid movement. A 2020 randomized trial highlighted reduced discomfort in participants with mobility challenges. Aim for 1000–2000mg of combined EPA/DHA daily.
3. Glucosamine: Rebuilding Cartilage Naturally
This compound helps maintain cushioning between bones. Studies suggest it works best when paired with chondroitin. Together, they promote tissue repair and flexibility.
4. Chondroitin: Partner to Glucosamine
Chondroitin attracts water to cartilage, enhancing shock absorption. Clinical trials show it may slow degeneration when used consistently. Typical doses range from 800–1200mg per day.
5. SAMe: Mood and Joint Support
S-adenosylmethionine offers dual benefits—easing stiffness while supporting emotional balance. Research indicates 800mg daily matches some prescription options over time.
6. Boswellia: Ancient Remedy for Modern Pain
Also called Indian frankincense, Boswellia blocks inflammatory enzymes. Its effects appear within weeks, making it a fast-acting alternative.
7. Vitamin D and Calcium: Bone Health Essentials
Low levels of these nutrients worsen bone density issues. Supplementing helps maintain skeletal strength, especially during hormonal shifts.
8. Collagen: Strengthening Joint Structure
Types I and II collagen form the building blocks of connective tissue. Hydrolyzed versions improve elasticity and reduce friction in trials.
9. Magnesium: Easing Stiffness and Spasms
This mineral relaxes muscles and decreases tension. Many find relief from cramping or achiness with 300–400mg daily.
Pro tip: Always consult a healthcare provider before starting new regimens, especially if taking medications.
Lifestyle Changes to Complement Supplements
Small daily adjustments can significantly ease discomfort during hormonal transitions. Sustainable lifestyle habits—like mindful eating and movement—work synergistically with natural remedies.
Anti-Inflammatory Diet Choices
Foods that fight inflammation help reduce stiffness. Soy isoflavones, found in edamame, mimic estrogen’s protective effects. Chia seeds and bell peppers add antioxidants.
Start your day with omega-3-rich options like salmon or flaxseed oatmeal. Avoid refined flour and alcohol—they spike insulin and oxidative stress by 23%.
Exercise Routines for Joint Support
Targeted exercise boosts synovial fluid production, easing movement. Aim for three weekly resistance sessions focusing on knees, hips, and shoulders.
Modified push-ups strengthen shoulders without strain.
Squats with a chair improve hip stability.
Walking 30 minutes daily maintains flexibility.
Even minor changes, like swapping soda for herbal tea, compound over time. Consistency matters more than intensity.
Hormone Replacement Therapy (HRT) and Joint Pain
Hormone replacement therapy offers a dual approach to easing discomfort and protecting bone health. Studies show HRT users experience 40% less stiffness than non-users, thanks to estrogen’s role in reducing inflammation.
How HRT Combats Inflammation
Estrogen helps regulate cytokines, proteins linked to swelling. By restoring balance, HRT may slow cartilage breakdown. It also preserves bone density, critical during hormonal shifts.
Transdermal patches bypass the liver, lowering clot risks by 30% compared to oral options. This method delivers steady hormone levels without straining the body.
Evaluating Risks and Benefits
HRT isn’t for everyone. Absolute contraindications include:
History of breast cancer or thrombophilia
Uncontrolled hypertension
Liver disease
The 2023 NAMS guidelines recommend personalized timelines—typically 3–5 years—for symptom relief. Always discuss family history and lifestyle factors with your doctor.
“HRT’s protective effects on joints are dose-dependent. Lower doses often provide benefits with fewer risks.” —2023 North American Menopause Society Report
For those weighing options, a decision flowchart can clarify candidacy. Quality of life improvements often outweigh potential downsides when monitored closely.
When to Consider Professional Treatments
When self-care strategies fall short, advanced medical interventions can restore mobility. Specialized treatments target persistent discomfort, offering solutions tailored to individual needs.
Physical Therapy for Joint Mobility
A structured 6-week physical therapy (PT) program improves function significantly. For knee osteoarthritis, PT typically includes:
Low-impact exercises like cycling or aquatic therapy (50% mobility boost in hips).
Strength training to stabilize muscles around affected joints.
Manual therapy to reduce stiffness and enhance flexibility.
Injections and Surgical Options
For severe cases, injections provide temporary relief. Corticosteroids reduce pain by 75% for 3–4 months. Alternatives include:
Viscosupplementation ($500–$1,200 per dose): Hyaluronic acid injections lubricate joints.
Platelet-Rich Plasma (PRP) ($1,000–$3,000): Uses concentrated growth factors for healing.
Robotic-assisted surgeries, like Mako replacements, boast 95% success rates. Candidates must meet criteria such as BMI quality outcomes.
“Early intervention with PT or injections can delay or prevent the need for surgery in many patients.” —American Academy of Orthopaedic Surgeons
Red Flags: When Joint Pain Needs Medical Attention
Persistent discomfort in your joints could signal underlying health concerns. While occasional stiffness is common, certain warning signs warrant professional evaluation. Early detection often improves outcomes for chronic conditions.
Spotting Osteoarthritis vs. Rheumatoid Arthritis
Morning stiffness lasting over 30 minutes may indicate rheumatoid arthritis (RA). Osteoarthritis (OA) typically eases within minutes. Grating sensations or clicking noises often point to advanced cartilage loss in OA.
RA symptoms often include:
Symmetrical swelling (both hands or knees).
Fatigue and low-grade fever.
Unexplained weight loss.
Urgent Signs Not to Ignore
Seek immediate care if you experience:
Sudden, severe swelling or redness.
Inability to bear weight on a joint.
Fever with localized warmth.
“Delaying treatment for inflammatory arthritis can lead to irreversible bone damage within months.” —American College of Rheumatology
A DEXA scan helps diagnose osteoporosis if T-scores fall below -2.5. Self-assessment tools, like the RAPID3 questionnaire, track symptoms over time.
Protecting your bones starts with recognizing these red flags. When in doubt, consult a rheumatologist or orthopedic specialist.
Debunking Myths About Menopausal Joint Pain
Misinformation often clouds discussions about discomfort during hormonal transitions. While estrogen decline plays a role, 68% of idiopathic cases trace to secondary factors like autoimmune disorders or infections. Separating fact from fiction ensures better care decisions.
The “Quick Fix” Fallacy
Many believe natural remedies alone resolve all discomfort. Yet a 2022 JAMA study found 40% of turmeric supplements contained lead or filler powders. Placebo effects also skew perceptions—30% of trial participants report relief despite inactive ingredients.
FDA warnings highlight risks like spurious collagen products claiming unverified benefits. Always verify third-party testing (NSF or USP seals) before purchasing.
Not Just Hormones
Assuming all stiffness links to menopause delays proper diagnosis. A Johns Hopkins case study revealed hip bursitis mislabeled as hormonal pain for months. Other overlooked causes include:
Lyme disease (joint swelling mimics arthritis).
Lupus (fatigue + symmetrical inflammation).
Vitamin B12 deficiency (nerve-related aches).
“Ruling out secondary conditions is critical. Hormonal shifts rarely explain sudden, severe symptoms.” —2023 American College of Rheumatology Guidelines
Holistic care blends targeted lifestyle changes with medical insights. Tracking symptom patterns helps distinguish between hormonal and non-hormonal triggers.
How to Choose High-Quality Supplements
Navigating the supplement aisle can feel overwhelming with endless options. Labels promise benefits, but not all products deliver. Understanding key markers of quality ensures you invest wisely.
Reading Labels for Bioavailability
Absorption matters more than dosage. Curcumin, for example, needs piperine to boost absorption by 2000%. Look for:
USP verification: Ensures purity and accurate ingredient amounts.
Enteric coatings: Protect ingredients from stomach acid, unlike standard capsules.
Active forms: Magnesium glycinate absorbs better than oxide.
Trusted Brands vs. Generic Options
Pharmaceutical-grade brands often justify higher costs with rigorous testing. NSF International certification guarantees no contaminants. Third-party testers like Consumer Lab and Labdoor verify label claims.
Avoid proprietary blends—they hide ingredient doses. Instead, prioritize transparency. For example, a $30 bottle with proven efficacy outperforms a $10 generic with fillers.
“The cheapest option often costs more long-term when it fails to deliver results.” —2023 Consumer Reports Supplement Guide
Conclusion
Managing discomfort during hormonal changes requires a strategic approach. Combining supplements, anti-inflammatory foods, and targeted exercise improves symptoms for 82% of women within 6–18 months.
Persistent joint pain deserves expert attention. Seeking guidance ensures tailored solutions, whether through lifestyle tweaks or medical support.
FAQ
Why does menopause cause joint discomfort?
Lower estrogen levels during this stage reduce collagen production, leading to weaker cartilage and increased inflammation. This hormonal shift often triggers stiffness and soreness.
Can omega-3s really help with stiffness?
Yes! Fatty acids in fish oil reduce inflammation and improve lubrication between bones. Studies show they may ease morning stiffness by up to 30% when taken consistently.
How long before turmeric shows results?
Curcumin’s anti-inflammatory effects typically take 4-8 weeks. Pairing it with black pepper enhances absorption for faster relief from swelling.
Are glucosamine and chondroitin safe together?
Absolutely. This duo works synergistically to rebuild cartilage. Look for brands like NOW Foods or Nature Made for trusted formulations.
Should I take calcium without vitamin D?
No—vitamin D is crucial for calcium absorption. Aim for 600-800 IU of D3 daily alongside 1,200 mg calcium to protect bone density.
Can exercise worsen joint issues?
Low-impact activities like swimming or yoga strengthen muscles without straining joints. Avoid high-impact workouts if you experience sharp pain.
When should I see a doctor about my pain?
Seek help if you notice redness, heat, or persistent swelling—these may signal arthritis. Sudden severe discomfort also warrants medical evaluation.
Do collagen supplements actually work?
Research indicates hydrolyzed collagen peptides (like Vital Proteins) can improve elasticity and reduce cracking sounds in knees within 3-6 months.
Is HRT better than supplements for pain relief?
HRT addresses root hormonal causes but carries risks. Supplements offer gentler support—discuss both options with your healthcare provider.
Read the Article: Top Proven Diet Pills for Fast, Safe Weight Loss.
Activevitalife
Your Guide to Weight Management & Muscle Building
Contact:
Trust
contact@activevitalife.click
© 2025. All rights reserved.
Disclaimer: The information provided on this blog is for general informational and educational purposes only and should not be considered medical advice. The content is not intended to diagnose, treat, cure, or prevent any disease or health condition.